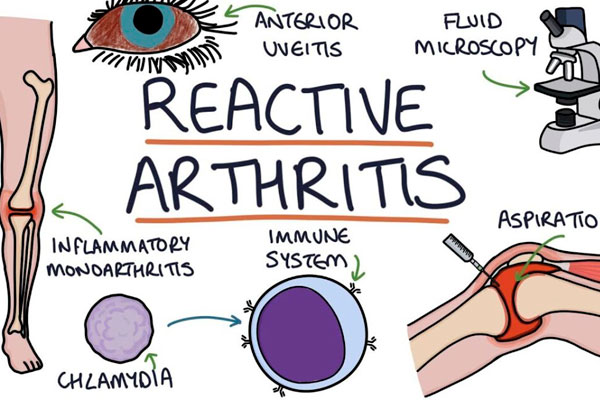
Did you know there are over one hundred different forms of arthritis? Some forms, like osteoarthritis and rheumatoid arthritis, are common enough that most people have at least heard of them. There are other forms that are not so common. One of them is reactive arthritis. This particular form of the disease is generally the result of bacterial infection.
Diagnosing reactive arthritis is difficult. As such, patients are frequently misdiagnosed until they eventually see a rheumatologist. As a consultant rheumatologist with the NHS, reactive arthritis patients are often referred to me. I can assure you that the disease, while uncomfortable, is rarely serious.
Inflammation: The Primary Symptom
GPs may have trouble diagnosing reactive arthritis because there are no specific lab tests to confirm it. The lab tests rheumatologists rely on only rule out other conditions, thereby allowing for a reactive arthritis diagnosis. The primary symptom we look for is inflammation.
By definition, arthritis is an inflammatory disease. Reactive arthritis fits the bill. It causes inflammation in the joints, particularly the knees, ankles, feet, and wrists. Inflammation can also appear in the tendons (tendinitis), bones (enthesitis), and spine (spondylitis).
Some reactive arthritis patients complain of pain in the lower back and buttocks. Others experience heel spurs and general pain in the heels.
A Bacterial Infection
The pain is always uncomfortable, but one of the encouraging things about reactive arthritis is that it is caused by a bacterial infection. Get rid of the infection and the arthritis symptoms go away. There are only a few types of bacteria that science has thus far linked to reactive arthritis:
- Chlamydia trachomatis
- Salmonella
- Shigella
- Yersinia
- Campylobacter
Chlamydia trachomatis is transmitted through sexual contact. It can enter the body through the vagina or urethra. The remaining four bacteria are transmitted through food. Thus, people stricken with food poisoning are at a greater risk of developing reactive arthritis.
Antibiotics and Rest
Treatment for reactive arthritis is fairly simple. If a patient still has the bacteria in their system, antibiotics will take care of it. As for the arthritis symptoms, these generally clear up over time. The best treatment for these is a combination of rest and moderate exercise.
Almost all cases of reactive arthritis resolve on their own. That being said, arthritis pain may continue for up to a year after the bacteria is eradicated. Most cases of long-term reactive arthritis pain are linked to pain in the lower back and buttocks.
Self-Care at Home
As a private rheumatologist, I may deem it appropriate to prescribe NSAIDs or corticosteroids to help manage reactive arthritis inflammation. In extreme cases, disease-modifying antirheumatic drugs may be needed to bring severe inflammation under control. But for the most part, the way to treat reactive arthritis is through self-care.
I recommend starting with a proper diet and ensuring that all food in your home is stored properly. You want to minimise the risk of reinfection through food poisoning.
Next, staying active is the best way to maintain joint flexibility until arthritis symptoms clear up. Moderate daily exercise is always appropriate. At night, making a point to get sufficient restful sleep only helps the body repair itself more fully.
If you believe you might be experiencing pain as a result of reactive arthritis, I am here to help. My private rheumatology clinic in London is always accepting new patients. You are more than welcome to schedule a visit at your earliest convenience.
How to prevent reactive arthritis
We all know that prevention is better than cure, so when it comes to reactive arthritis, you can do a lot to help prevent yourself from having it again.
The most effective way to prevent reinfection is to avoid the most common causes of reactive arthritis as much as possible. These include avoiding:
- Infections of the bowel and digestive system (gastrointestinal infections)
- Sexually transmitted infections (STIs)
The proper use of barrier contraception such as condoms during sexual intercourse is the most effective way to avoid contracting an STI. Using condoms will significantly reduce your risk of getting and spreading STIs, such as gonorrhoea and chlamydia. These are the two most common types of STIs that can trigger reactive arthritis.
Good food hygiene practices
Food poisoning is one of the most common causes of reactive arthritis. This is why it can help you avoid developing the condition by following good food hygiene practices in the home to help prevent gastrointestinal infections that can lead to reactive arthritis.
Here are some simple yet effective tips to help maintain good food hygiene levels in your home:
- Wash your hands with soap and hot water before and after handling food
- Wash your hands with soap and hot water after going to the toilet
- Use a disposable tissue to blow your nose and wash your hands afterwards
- Wash your hands after touching pets
- Clean your kitchen work surfaces and chopping boards with an anti-bacterial cleaner before and after preparing food
- Use separate chopping boards to prepare raw meat and fish and cooked foods
Wash raw salads thoroughly in cold water before consuming: According to research by Leicester University, bagged salad can fuel the growth of food-poisoning bugs like Salmonella. Fresh green leaves and salad foods are often involved in food poisoning.
Experts recommend that you eat bagged salads on the day of purchase to prevent bacterial growth within the bag. Keeping your fridge temperature between 0-5ºC (31.9-40.9ºF) and keeping food cold will help to prevent bacteria from rapidly growing.
Article by Dr. Naveen Bhadauria