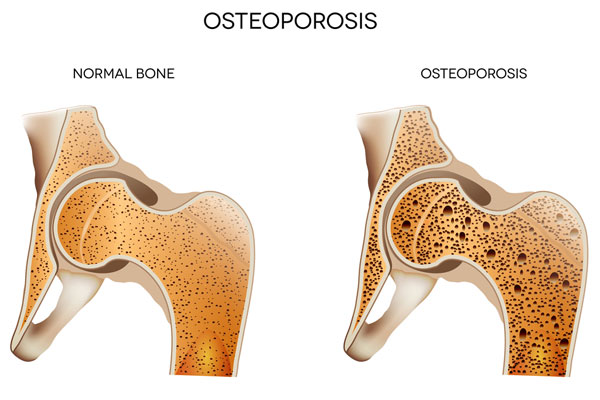
It has been estimated that some 3 million people in the UK suffer from osteoporosis. It is often called the ‘silent disease’ because people don’t know they suffer from it until a fracture resulting from a fall reveals it. Osteoporosis is a degenerative condition that gradually weakens bones and makes them more brittle over time. That’s why people with the disease are more prone to fractures.
As a private rheumatology consultant in London, I consult with osteoporosis patients on a regular basis. I am happy to say that there are a number of treatments we can utilise to help patients continue living full lives even with this disease. Know that in every case, treatments are recommended after considering a number of factors, including:
- age and sex
- previous medical history
- the risk of additional fractures
Fracture risk is especially important if you are only diagnosed with osteoporosis after suffering a fracture. Your treatment would likely include strategies for preventing broken bones in the future.
Dietary Changes
The first course of treatment may involve nothing more than dietary changes. As we age, the body does not make the best use of the foods we eat. Therefore, treating osteoporosis may involve changing the way you eat so as to increase the amount of calcium and vitamin D you are getting.
Your doctor may ask you about your regular eating habits. If necessary, he or she may recommend trying other foods. If your diet is already where it should be, your doctor may recommend calcium and vitamin D supplements.
Treatments for Osteoporosis Options
1. Medications: Several types of medications are approved by the National Institute for Health and Care Excellence (NICE) in the UK to prevent and treat osteoporosis.
- Bisphosphonates: These include alendronic acid (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Aclasta). Bisphosphonates are typically the first line of treatment for osteoporosis and work by slowing down bone loss. Bisphosphonates are available in four common medications and are administered either orally or by way of injection. The two biggest downsides to these medications are that they can take up to a year before measurable results are observed and you may have to take them for five years or longer.
- Denosumab (Prolia): This is a monoclonal antibody that inhibits a protein involved in bone breakdown. It is used in postmenopausal women at high risk of fractures and men at increased risk due to other underlying conditions or steroid use.
- Selective estrogen receptor modulators (SERMs): Raloxifene (Evista) is a SERM that mimics the beneficial effects of estrogen on bone density without some of the risks associated with estrogen. It is used primarily in postmenopausal women.
- Parathyroid hormone analogues: Teriparatide (Forsteo) and abaloparatide (Tymlos) are drugs that help to stimulate new bone formation. They are typically reserved for those with severe osteoporosis who have had multiple fractures.
2. Calcium and Vitamin D Supplements: These supplements are typically recommended alongside other osteoporosis medications to ensure that there is enough calcium and vitamin D for bone health.
3. Lifestyle Changes: Diet and exercise play a critical role in managing osteoporosis.
- Diet: Consuming a balanced diet rich in calcium and vitamin D is essential for bone health. Dairy products, green leafy vegetables, and fortified foods are good sources of these nutrients.
- Exercise: Regular physical activity, especially weight-bearing and muscle-strengthening exercises, can help improve bone density and strength. It also improves balance and coordination, reducing the risk of falls and fractures.
Lifestyle changes may be recommended depending on the severity of the disease. If a patient’s bones are especially brittle, doctors may recommend avoiding terribly strenuous activity until bone density increases sufficiently. At the same time, moderate, low impact exercise can be helpful. Doctors will help patients find that perfect balance.
Patients engaging in risky activities that could result in fractures are generally advised to set those activities aside, at least temporarily. If bone density does not recover, such activities may have to be abandoned altogether.
Osteoporosis is a fairly common disease. Although it mainly affects older people, younger patients are seen from time to time. If you think you might be suffering from osteoporosis, I am available to work with you and help you figure it out. Make an appointment to meet with me in my London clinic at your earliest convenience.
4. Fall Prevention: Simple measures can significantly reduce the risk of falls at home, such as removing tripping hazards, using non-slip mats, and installing grab rails in necessary areas.
5. Hormone replacement therapy (HRT): While not a first-line treatment for osteoporosis, HRT can be used to relieve menopausal symptoms and can also help to improve bone density.
Changes in hormone production are generally a contributing factor to osteoporosis. Therefore, other treatments are based on restoring hormonal balance. A doctor may recommend a parathyroid hormone designed to increase bone density by encouraging more calcium production.
Female patients may be advised to consider selective oestrogen receptor modulators (SERMs). These medications mimic the actions of the natural oestrogen hormone. Likewise, doctors may recommend hormone replacement therapy to female patients. Testosterone may be suggested to male patients.
Final Words
The choice of treatment for osteoporosis in the UK is individualised based on the patient’s age, sex, risk of fractures, and the presence of other health conditions. It’s important to discuss the benefits and risks of these treatments with your healthcare provider to determine the best strategy for you. With effective management, individuals with osteoporosis can lead active, healthy lives.
Article by Dr. Naveen Bhadauria